Abstract
Background: The cumulative red blood cells (RBC) transfusion burden is known to impact outcomes in myelodysplastic syndromes (MDS) but doesn't accurately predict prognosis during the early disease phase. Here we aimed to assess the prognostic value of early changes in transfusion patterns in addition to the recent IPSS-M scoring system.
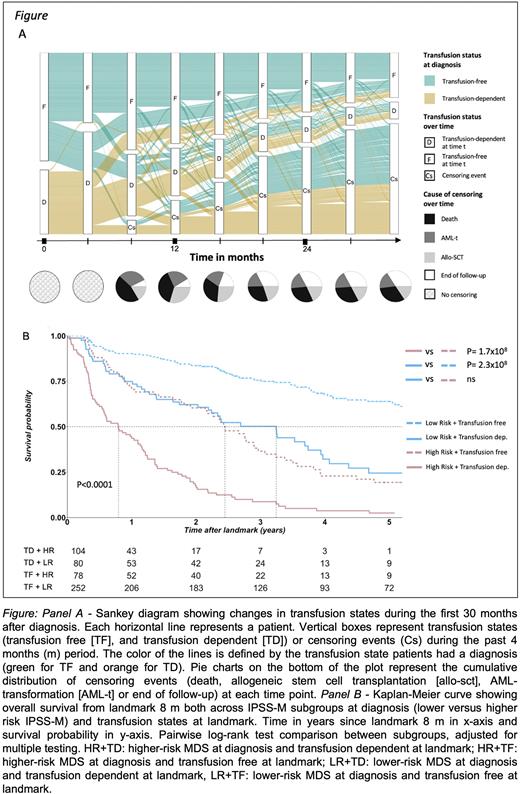
Methods: We gathered diagnostic biobank samples from adult patients (pts) with MDS and registered in the Karolinska Institute's biobank (KI) and the National Swedish MDS Biobank (NB) between 2003-2017 and 2013-2017, respectively. DNA targeted sequencing (152 genes) was performed (Bernard et al., NEJM Evid, 2022). Clinical data was retrieved through pts’ charts (KI) and the Swedish cancer registry (NB). Pts were treated according to Nordic/EU guidelines and most common therapies for lower-risk MDS and higher-risk MDS were erythropoietin and azacytidine, respectively. Transfusion data was obtained from the SCANDAT registry. Pts were followed with regards to RBC transfusion until censored due to death, transformation to acute myeloid leukemia (AML-t), allogenic stem cell transplantation (allo-SCT), or end of follow-up on the 31st of August 2018, whichever occurred first. As per the IWG hematological response criteria for MDS (Platzbecker et al., Blood 2019), transfusion states (TS) were categorized every 4 months (m) as transfusion dependent (TD) or transfusion free (TF) during the past 4 m period. Lower-risk MDS (LR) was defined as IPSS-M very low, low and moderate low, and higher-risk MDS (HR) as IPSS-M very high, high and moderate high at diagnosis (Bernard et al., NEJM Evid, 2022). Landmark analyses of overall survival (OS) were performed with the Kaplan-Meier method for estimating probabilities of OS over time. Multivariable analyses were conducted using Cox proportional hazards model.
Results: We gathered a cohort of 688 pts with MDS from KI (n=424) and 33 other clinics in Sweden (NB, n=264). Median age at diagnosis was 74 years (y) old (range 19-93). The male:female ratio in the cohort was 1.4. At diagnosis, 63% of the pts were TF. Out of 646 pts evaluable by the IPSS-M score at diagnosis 54% had LR. Most frequently mutated genes in the cohort were TET2, SF3B1, ASXL1, DNMT3A, RUNX1, TET2, TP53 (66% TP53 multihit), U2AF1, STAG2, ZRSR2. Changes between TS (transitions) preferentially occurred within a year after diagnosis (panel A) with a median time for occurrence of transfusion-related transitions of 1.0 y (range 0.33-8.37). Based on this finding, we assessed whether TS at 8 m landmark impacted prognosis. We observed that there was a significant difference in OS since landmark between TF pts compared with TD pts at landmark 8 m and across IPSS-M categories (panel B). LR pts who were TD at 8 m, had a median OS of 3.2 y (95% CI: 2.2-4.0) versus 6.9 y (95% CI: 5.6-8.9) for LR pts who were TF (P<0.0001). Similarly, median OS was 0.8 y (95% CI: 0.6-1.1) in HR and TD pts while it was 2.4 y (95% CI: 2.1-3.1) in HR and TF pts at landmark 8 m (P<0.0001). Interestingly, OS for LR pts who were TD didn't significantly differ from HR pts who were TF at 8 m. Overall, pts TD at 8 m had more gene mutations compared to TF pts (median 5 [1;13] and 4 [1;16], respectively, P=0.0084). Moreover, studying specific genetic subgroups of MDS, TS at 8 m distinguished subsets of pts with adverse or favorable outcomes within SF3B1-mutated LR pts. In this population, the median OS in pts TF at 8 m was 8.4 y (95% CI: 6.5-13.1) compared to 3.2 y (95% CI: 1.7-4.1) for TD pts (P<0.0001). Next, in multivariable analysis, we found that TD at 8 m significantly impacted OS (HR=2.4 [95% CI: 1.9-3.1]), independently of diagnostic IPSS-M score, age, gender and type of MDS (de novo or therapy-related).
Conclusion: TS at landmark 8 m, usually after outcome of first-line treatment was evaluated, appears to be a strong and independent predictor of OS in MDS. These findings are of particular importance for the LR group in which it could discriminate subsets with favorable outcomes from those with adverse prognosis. In addition to the IPSS-M calculation at diagnosis, transfusion dependency could be easily used for prognostic reassessment during follow-up. More generally, these results highlight the need of dynamic outcomes prediction tools and/or validation of current prognostic scores in dynamic settings. Finally, multistate modeling of the dataset is being completed and aims to assess how changes of transfusion patterns over time impact prognosis.
Disclosures
Bernard:Pfizer: Honoraria. Nilsson:Celgene/BMS: Honoraria; Novartis: Honoraria. Papaemmanuil:Isabl Inc.: Current equity holder in private company, Current holder of stock options in a privately-held company, Other: CEO, Patents & Royalties: Whole genome cancer analysis; TenSixteen Bio: Current equity holder in private company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal